Why Choose Us?
0% AI Guarantee
Human-written only.
24/7 Support
Anytime, anywhere.
Plagiarism Free
100% Original.
Expert Tutors
Masters & PhDs.
100% Confidential
Your privacy matters.
On-Time Delivery
Never miss a deadline.
PLEASE PAY ATTENTION TO THE SCENARIO AND THE SAMPLE ESSAY ATTACHED
PLEASE PAY ATTENTION TO THE SCENARIO AND THE SAMPLE ESSAY ATTACHED.ZERO PLAGIARISM FIVE REFERENCE NOT MORE THAN 5 YEARS NOTE: Patient is 59 years old African American male who was admitted to the long
Running head: COMPREHENSIVE CLIENT ASSESSMENT 0
Comprehensive Client Assessment
Student name
Walden University
NURS 6640, Section 9, Psychotherapy with Individuals
December 15, 2019
Comprehensive Client Assessment
Psychiatric mental health nurse practitioners (PMHNPs) provide care to clients with mental health disorders and substance use disorders who may be in vulnerable states during their initial contact with the PMHNP, when they seek treatment. No single approach to mental health treatment is suitable for all clients, and it is critical for the PMHNP to conduct a thorough assessment to accurately diagnose each client and determine which treatment approach is most likely to enhance the client’s clinical outcomes (American Nurses Association, 2014; Ball, Dains, Flynn, Solomon, & Stewart, 2018; Marcogliese & Vandyk, 2019; McAllister, Happell, & Flynn, 2014; Wheeler, 2014). A comprehensive client assessment should be performed by the psychiatric mental health nurse practitioner during a client’s initial appointment, to facilitate formulation of an appropriate, client-centered treatment plan. A comprehensive client assessment engages the client in their treatment plan, establishes rapport and contributes to a therapeutic alliance between the practitioner and the client, and collects information about the client to facilitate development of a compassionate understanding of the client, an accurate diagnosis, and an appropriate client-centered treatment plan (Ball et al., 2018; Wheeler, 2014). The purpose of this assignment is to assess a client presenting for psychotherapy and to develop a genogram for the client, to gather the information needed to make an informed diagnosis and to formulate an appropriate client-centered treatment plan that will enhance client outcomes.
Demographic Information
The client is a 23-year-old Caucasian male who speaks English and who resides with his parents and his youngest brother in their home in a coastal town in New England. The client has never been married and does not have any children. The client identifies as Christian. The client identifies as a straight male. The client is covered via Blue Cross Blue Shield, under his parents’ health insurance. The client’s father owns his own real estate and contracting business and his parents are upper-class residents of a coastal town in New England and own a second, winter-home, in one of the southern states. The client arrived to his appointment via his vehicle, which he says he owns.
Presenting Problem
The client reports “anger outbursts and mood swings for my whole life” and issues with alcohol consumption.
History of Present Illness
The client describes a several-year history of anger outbursts and mood swings, beginning when he was approximately eight-years-old, and occurring multiple times per week. The client reports that in the past, during angry outbursts, he has behaved in a destructive manner, punching holes in walls, throwing objects, slamming doors, and once he smashed something with a baseball bat. With the exception of a recent assault charge related to an explosive angry outburst while under the influence of alcohol, the client denies any other history of physical violence or aggression towards people, but reports frequent verbal aggression. The client reports his explosive outbursts have caused him problems in his interpersonal relationships. The client denies getting into frequent physical altercations as a child and denies cruelty to animals. The client reports episodes of road rage. The client also describes an increased pattern of alcohol consumption. The client reports his anger outbursts and alcohol consumption contributed to an incident within the past month in which he got in argument with his girlfriend, became angry and agitated, then pushed a neighbor, broke a sliding glass door and screen, and pulled a fire alarm, resulting in his arrest. The client was charged with assault and battery, disorderly conduct, and falsely alerting the fire department. The client says he spent 30 hours in jail following his arrest. The client reports his mood is variable and endorses some history of hypomanic episodes, but says they never last longer than one or two days. The client reports a history of non-suicidal, self-injurious behavior including cutting as a teenager and head banging and denies current self-injurious behavior. Client reports occasionally experiencing suicidal thoughts but denies suicidal plan or intent and has no history of suicide attempts. The client reports his sleep is okay but he says he sometimes wakes up early in the morning with anxiety, a racing heart, and heartburn. The client reports using guided meditation to help with his anxiety. The client hopes to address his anger issues and alcohol consumption to reduce the incidence of angry outbursts and prevent further interpersonal problems and problems with the law.
Past Psychiatric History
The client has a history of angry outbursts, mood swings, and mood fluctuations with brief periods of hypomania. The client also reports feeling depressed at times, with a history of self-injurious behavior, and more recently, increased alcohol consumption. The client denies periods of depression lasting longer than a few days. In 2018, the client was prescribed bupropion (Wellbutrin) 150 mg orally, twice a day, by his primary care provider. The client reports the bupropion (Wellbutrin) improved his mood but was ineffective for reducing his angry outbursts. The patient reports a trial of escitalopram last spring and says it was ineffective for his mood and anxiety even at a dose of 20 mg orally per day. The patient also reports a trial of lamotrigine, which he says his aggression did not respond to, so he says it was discontinued after a month. The client reports seeing a therapist for counseling for six months when he was 17. The client has no history of psychiatric hospitalizations. The patient denies any other history of abuse or trauma.
History of Abuse or Trauma
The client reports a long-standing history of verbal abuse by his father, which he reports has gone on for as long as he can remember and continues, to this day. The client says his father demeans him, calls him names, insults, and embarrasses him in front of other people. The client reports some history of physical abuse by his father but declines to go into detail, at this time, reporting that the abuse was never severe enough to require medical attention. The client denies recent physical abuse by his father and says this has not happened since he “was a kid”.
Medical History
The client reports a history of irritable bowel symptoms, which he says are influenced by his mood, with angry outbursts and anxiety contributing to irritable bowel symptoms. The client’s annual physical assessment was unremarkable, with the exception of a documented history of irritable bowel syndrome. The client reports he is up to date with his immunizations, gets an eye exam every two years, gets a dental cleaning every year, and says he does self-testicular exams. The client’s vital signs are within normal limits, as noted below, his height is 5’11”, his weight is 150 pounds, he has an athletic build, and his body mass index is 20.9. The client reports an allergy to nickel but denies any drug or food allergies. The client’s current medications and supplements are as follows: fish oil supplement, amino acid supplement, multivitamin, melatonin, probiotic, omeprazole, and peppermint oil. The client reports a history of banging his head against the wall during angry outbursts but denies any injuries or loss of consciousness related to this behavior. The client denies any hospitalizations, surgical history, or significant injuries. Collecting a client’s medical history is important when assessing and diagnosing the client for a mental health disorder, as research suggests medical conditions can cause symptoms of mental health disorders, such as mood fluctuations and anxiety, and mental health disorders can cause symptoms of medical conditions, such as heart palpitations and indigestion (Zolezzi, Abdulrhim, Isleem, Zahrah, & Eltorki, 2017).
Substance Use History
Clients reports his alcohol consumption began socially, when he was 17, at which time he would drink five to six drinks approximately two times per month. Client reports his alcohol consumption increased and has become problematic and resulted in him acting out and getting in trouble with the law. He reports his most recent binge drinking episode of alcohol consumption consisted of three mimosas, four tequila shots, which he says he consumed before two o’clock in the afternoon. Client reports his last alcohol consumption was approximately one week ago, during the above incident. The client also reports using marijuana every day or two, multiple times per day, over the past four years, which he says helps with his anxiety. The client reports his last marijuana use was approximately one week ago. The client denies ever using amphetamines, bath salts, benzodiazepines, methamphetamine, ecstasy, heroin, phencyclidine, spice, methadone, narcotics, or nicotine. The client denies caffeine use and denies the use of any other substances. Mental health disorders can influence cravings and contribute to substance use disorders, and substance use disorders can contribute to symptoms of mental health disorders, such as depression, anxiety, mania, and angry outbursts (Serre, Fatseas, Swendsen, & Auriacombe, 2017). Research by Coccaro et al. (2016) suggests persons with an impulsive disorder such as intermittent explosive disorder are at a increased risk of developing a substance use disorder when compared to persons with impulsive disorders.
Developmental History
The client is not accompanied by either of his parents during this appointment, but reports, to his knowledge, his mother’s pregnancy with him was uneventful, she did not use any substances during this pregnancy, he was born via a vaginal birth at full term, and weighed “around seven pounds”. The client reports he reached all of the expected developmental milestones on time. He says he walked by 10 months, spoke in full sentences and was potty-trained by two-and-a-half, and began preschool at age three. The client does not recall any history of separation anxiety when he began preschool. The client says he excelled throughout elementary, middle, and high school and graduated with honors. The client says he was active and excelled in sports throughout elementary, middle, and high school, including baseball. The client says his father coached his baseball team and set very high expectations for his performance in sports and his academic performance when he was growing up. The client reports healthy relationships with all of his siblings growing up, with a normal amount of sibling rivalry, and says he was and still is closest to his sister. The client reports having a girlfriend, who he says he has been dating for over three years, and reports a healthy sexual relationship with her. The client reports completing three years of college with a major in engineering, but he says he left college to work for his father’s residential real estate business.
Family Psychiatric History
The client is the oldest of four children and says his sister, who is 22, has a mood disorder for which she is prescribed bupropion (Wellbutrin) and he says she does not have a substance use disorder. The client says, to his knowledge, his 20-year-old brother and 16-year-old brother have no history of mental health or substance use disorders. The client reports his mother, who is 44, is healthy and has no history of mental health disorders or substance use disorders. The client reports his father, who is 48, has bipolar disorder with mood instability and angry outbursts. The client says his father has one brother, who is 44, who has a mood disorder and a substance use disorder, is addicted to heroin, and has been in and out of jail. The client says his paternal grandfather, who is in his late sixties, is a chain smoker and has a mood disorder, and says he is mean and has frequent mood swings and angry outbursts. The client reports his paternal grandfather’s father, the client’s great grandfather, also had a mood disorder, and the client says he died at the age of 78, “from natural causes”. The client reports his paternal grandfather’s mother, the client’s great grandmother, is healthy and has no substance use disorders or mental health disorders. The client reports his paternal grandmother and paternal grandmother’s parents, his great grandmother and great grandfather, are all healthy with no know substance use or mental health disorders. The client reports his mother has two younger sisters and one younger brother, whom, to his knowledge, are all very healthy and do not have substance use or mental health disorders. The client reports he does not know his maternal grandfather, who he says is in his late sixties and is divorced from his maternal grandmother, but he reports his maternal grandfather has alcohol use disorder. The client reports that, to his knowledge, his maternal grandfather’s father, his great grandfather, was an alcoholic, and his maternal grandfather’s mother, his great grandmother, was healthy and had no substance use or mental health disorders. The client reports his maternal grandmother and his maternal grandmother’s father, his great grandfather, is healthy mentally and physically and does not have any substance use or mental health disorders. The client reports his maternal grandmother’s mother, his great granmother, does not have any substance use or mental health disorders but he says she has diabetes, has had strokes, and does not look after her physical health. Please refer to the appendix for the client’s family genogram. Research by Coccaro (2010, 2018), Mason, Brown, and Croarkin (2016), and Post et al. (2015), suggest persons with a multigenerational history of mood disorders such as bipolar disorder, impulsive disorders such as intermittent explosive disorder, and substance use disorder, have a greater incidence of mental health and substance use disorders.
Psychosocial History
The client was born and raised by in the same coastal, New England town where he lives today, by both of his biological parents, whom he still lives with. The client is the oldest of four siblings, with a 22-year-old sister, a 19-year-old brother, and a 15-year-old brother. The client says his youngest brother is the only other sibling living with him and his parents, at this time. The client reports he is a high school graduate and completed three years of college at the University of Rhode Island with a major in engineering and played division one baseball all three years he was in college. The client says he left college to work for his father’s residential real estate business. The client says he is a car enthusiast and says he owns his own vehicle. The client is in a long-distance relationship with his girlfriend of three years, whom he says lives in the Midwest but has discussed moving to New England to live with the client, and has been looking at apartments that they could share. The client says “I think it is a good thing. Yeah, it is a good thing!”. The client reports having good family supports and having a good relationship with his mother, his siblings, and his maternal grandparents and his paternal grandmother, but he says he has a difficult relationship with his father, who has angry outbursts and mood instability. The client reports he has a couple of good friends who are supportive. The client reports legal problems, as described above, including charges for assault and battery, disorderly conduct, and falsely alerting the fire department. He is court ordered not to drink alcohol and claims he has successfully refrained from consuming alcohol for the past week.
Review of Systems
Constitution
Client denies any recent unexplained weight gain or weight loss and reports his appetite is good. Client reports his sleep is okay and he averages approximately eight hours of sleep per night. Client denies weakness, fever, night sweats, and fatigue.
Head and Neck
No loss of consciousness, headaches, or fainting. Reports he used to bang his head against the wall, as a child, when he was angry, but denies injury related to this behavior. Denies history of injury or trauma to his neck. Client’s head is symmetrical and normocephalic. Client reports full range of motion to head and neck.
Chest
Client denies pain, skin changes, lumps, or discharge.
Eyes
Client denies vision problems and denies any recent changes in vision. Client does not wear glasses or contacts and reports he gets an eye exam every two years.
Ears
Client denies hearing problems and denies any recent changes in hearing. No changes in hearing, trouble hearing, or tinnitus. Client denies pain or discharge from ears.
Nose
Client reports an intact sense of smell. Client denies alterations in his sense of smell, nosebleeds, or sinus congestion.
Throat and Mouth
Client reports healthy teeth and gums and denies difficulty chewing, swallowing, or hoarseness. Client reports he gets his teeth cleaned annually.
Respiratory
Client denies respiratory issues such as cough, sputum, hemoptysis, and dyspnea while resting or during exercise. Client denies ever having tuberculosis and denies abnormal chest x-rays. Normal respiration rate and rhythm noted.
Cardiovascular/Peripheral Vascular
Client denies tachycardia or abnormal rhythm. Client reports episodes when it feels like his heart is racing, occurring during bouts of anxiety. Client denies chest pain while at rest or while exercising. Client denies peripheral vascular issues such as swelling in his legs or feet and pain with walking.
Gastrointestinal
Client reports a history of irritable bowel syndrome and occasional heartburn, for which he says he takes omeprazole. Client reports trying an elimination diet in the past but says he is no longer using this diet. Client reports he normally has bowel movements daily, with more frequent bowel movements during irritable bowel syndrome flareups. Currently, client denies recent changes in bowel habits and denies heartburn, nausea, vomiting, diarrhea, constipation, and abdominal pain.
Genitourinary
Client reports normal urinary pattern and denies increased urinary frequency, urgency, dribbling, hematuria, dysuria, incontinence, or waking at night to urinate. Client denies pain on either side of his lower back. Client reports completing monthly self-testicular exams and denies any abnormal findings.
Musculoskeletal
Client denies limits to his range of motion and denies any history of muscular or skeletal injuries. As noted above, client says he used to bang his against the wall and also says he has been in physical altercations but he denies any muscular or skeletal injuries related to this behavior.
Skin
Client denies skin issues such as rashes, bruises, lesions, and pruritis.
Hematologic
Client denies bleeding or bruising easily and denies any history of anemia.
Endocrine
Client denies increased thirst, increased urinary frequency, intolerance to heat or cold, changes to his hair, and any other endocrine symptoms. Client denies thyroid issues.
Allergic/Immunologic
Client denies any allergies or immune deficiencies.
Psychiatric
Client denies issues with sleep or changes in his appetite. Client reports a history of explosive, angry outbursts since he was eight, variable mood, with some history of hypomanic episodes, and more recent episodes of anxiety. Client reports a history of non-suicidal, self-injurious behavior through cutting and head banging and denies current self-injurious behavior. Client reports occasionally experiencing suicidal thoughts but denies suicidal plan or intent.
Neurological
Client denies a history of traumatic brain injury and denies dizziness, syncopal episodes, seizure activity, headaches, weakness, tingling, numbness, tremors, changes in gait, or loss of coordination. Client denies difficulty concentrating or changes in his memory.
Physical Assessment and Neurological Examination
A head-to-toe physical assessment of the client was not completed during this visit. The client’s annual physical assessment was unremarkable, with the exception of a documented history of irritable bowel syndrome. The client’s height is 5’11”, his weight is 150 pounds, and his body mass index is 20.9, which is within the normal range for a 23-year-old male. The client’s resting pulse is 68, his respirations are 16, blood pressure is 110/70, and his temperature is 98°F. The client reports he takes omeprazole for his gastrointestinal issues, which he claims is effective and he denies any gastrointestinal symptoms today.
roid insufficiency with mental disorder
Laboratory and Diagnostic Testing
While there is no specific lab work that can diagnose mood disorders or impulse control disorders such as intermittent explosive disorder, it is important to do comprehensive laboratory testing to rule out medical conditions and substance use, both of which can contribute to symptoms of mental health disorders (Serre et al., 2017; Zolezzi et al., 2017). A urine screen was completed and was negative for all substances, including opiates, buprenorphine, oxycodone, methadone, propoxyphene, barbiturates amphetamines, methamphetamines, benzodiazepines, cocaine, THC, and alcohol byproducts. Lab work was completed for this client that included a complete blood count with differential, hepatic panel, electrolytes, and blood urea nitrogen, all of which were within the normal range. The client’s thyroid levels were also checked, as research supports a connection between thyroid insufficiency and mental health disorders, such as mood disorders and anxiety (Kamble, Nandedkar, Dharme, L, & Bhosale, 2013; Pagana & Pagana, 2018).
Mental Status Exam
Appearance
Client’s appearance is congruent with his age. He has an athletic build and is neatly groomed and casually dressed, wearing a plaid shirt, jeans, a baseball cap, and boots.
Attitude
Client is calm and cooperative toward interviewer throughout assessment, makes appropriate eye contact, and engages appropriately throughout interview.
Behavior and Psychomotor Activity
Normal gait noted. Client sits up straight in chair with good posture, makes appropriate eye contact with interviewer, and does not shift, fidget, or leave his seat during the interview. Client is attentive and participates appropriately in exercises such as circle breathing.
Speech and Language
Client speaks clearly, coherently, and fluently, and uses language appropriate for his age, ethnicity, education level, and the context. Client’s speech is within normal limits for rate, tone, rhythm, volume, and cadence
Mood and Affect
Client reports his mood is “good”. Client’s affect is euthymic, thus is within a normal range and is congruent with his mood.
Temperament
Perception
No perceptual disturbances noted or reported. Perception is negative for any hallucinations or illusions.
Thought Process
Client’s thought process is logical and organized, and his stream of thought is linear and coherent.
Content of Thought
The client’s content of thought is negative for any suicidal or homicidal ideation, intent, or plan, and is negative for any delusional or other psychotic material. No obsessions, or preoccupations noted or reported.
Intelligence / Fund of Knowledge
The client’s knowledge level is appropriate for his age and educational level.
Sensorium
Client is alert and oriented to time, person, place, and event.
Cognition
Attention and Calculation: Client is attentive and can spell the word “world” forward and backward. Client can count backward from 100 using serial sevens.
Memory, Concentration, Registration, and Recall: Client’s memory and concentration are intact. Client’s short-term memory, long-term memory, and recall intact. Client recalls events from his childhood without difficulty. Client recalls what he ate for supper last night. Client’s registration intact, as evidenced by his success repeating three words back to interviewer immediately, “velvet, church, daisy”. Client’s recall is intact, as evidenced by the correct recollection of the three words, “velvet, church, daisy”, after five minutes.
Language: Client names items in the room appropriately, follows simple commands, and can draw a genogram.
Abstract Reasoning
Client demonstrates abstract reasoning. When asked what the unifying theme is between a bicycle, a plane, a train, and a car, the Client replied, “they are modes of transportation”. When asked how the following items are similar, “a chair, a night stand, a bookshelf”, the client replied, “they are all furniture”.
Insight and Judgment
Client’s insight and judgment are fair. He is aware of a problem with his behavior, and describes an angry outburst that got him in trouble with the law, but he is unsure of the type of help needed to address the problem. The client reports his behavior can be problematic when he drinks, but reports he drank too much alcohol despite recognizing this, and got into trouble with the law.
Differential Diagnosis
Intermittent Explosive Disorder (IED)
According to APA (2013), IED is an impulse control disorder associated with anger-based or impulsive aggressive outbursts that have a rapid onset and typically last up to 30 minutes. The client’s history indicates he meets the following diagnostic criteria for IED: Verbal aggression or physical aggression toward property or other individuals occurring, on average, twice weekly for a period of at least three months. Three behavioral outbursts involving damage or destruction to property or physical assault of other individuals occurring within a 12-month period. Additionally, the magnitude of aggression of the client’s most recent outburst was grossly out of proportion to the disagreement he had with his girlfriend, resulting in impulsive assaultive and destructive behaviors and resulting in legal consequences. As described above, the client’s history suggests he meets the diagnostic criteria for IED (APA, 2013). According to APA (2013), bipolar disorder and substance use disorder are associated with IED.
Alcohol Use Disorder (AUD), Moderate
According to APA (2013), AUD is a problematic pattern of alcohol use associated with two or more of the 11 symptoms of AUD, and associated with significant impairment or distress of the patient. Moderate AUD, includes the presence of four to five of the 11 symptoms of AUD. The client reported consuming alcohol in larger amounts and for longer periods than intended over the past year with a great deal of time spent using alcohol and recovering from its effects, consistent alcohol use despite having recurrent interpersonal, social, and behavioral problems exacerbated by the effects of alcohol, and continued alcohol use despite having a mental health disorder that is exacerbated by alcohol. The patient’s pattern of alcohol use and recent binge drinking episode resulting in his arrest support a diagnosis of moderate AUD (APA, 2013).
Bipolar Disorder, Unspecified, With Anxious Distress
According to APA (2013), while a diagnosis of Bipolar II disorder requires a history of at least one distinct hypomanic period lasting four or more consecutive days and a history of a major depressive episode lasting two weeks or longer, unspecified bipolar disorder does not require hypomanic episodes lasting four days or major depressive episodes lasting two weeks (APA, 2013). Aggressive outbursts, such as those described above, can also be related to bipolar disorder. The patient experienced feeling keyed up or tense and feeling like he might lose control of himself during anxious, hypomanic episodes, which are APA (2013) criteria for this diagnosis. The client’s mood fluctuations beginning in childhood, episodes of depression and hypomania, and multigenerational mood disorder support a diagnosis of bipolar disorder (Mason et al., 2016).
Case Formulation
The client is a 23-year-old Caucasian male with a history of mood swings, non-suicidal self-injurious behavior such as head-banging and cutting, and impulsive, explosive, angry outbursts since the age of eight, occurring multiple times per week, and associated with destructive and disruptive behavior such as punching holes in walls, throwing things, slamming doors, and smashing things with a baseball bat. The client also has an increasing pattern of alcohol use over the past six years, which he associates with exacerbating his mood swings and explosive outbursts. The client reports his explosive outbursts cause problems in his interpersonal relationships and more recently, following a binge-drinking episode, resulted in legal consequences. The patient is prohibited by law from consuming alcohol, and has maintained his sobriety for the past week but reports increased anxiety. The client has a multigenerational history of mood disorders and substance use disorders and claims his father also has frequent, unprovoked, explosive outbursts and exhibits symptoms of IED. Based on the comprehensive client interview conducted, this client meets the APA (2013) diagnostic and statistical manual of mental disorders fifth edition diagnoses for intermittent explosive disorder (312.34) and alcohol use disorder, moderate (303.90). While the patient has a family history of and demonstrates some symptoms of bipolar disorder, the patient will be monitored for symptoms of this disorder, throughout treatment, but does not meet the full criteria for this diagnosis, at this time, and neither antidepressant trial was associated with hypomanic or manic episodes (APA, 2013).
Treatment Plan
The client is seeking to maintain his sobriety and to control his angry outbursts and associated anxiety, and ultimately, to prevent further interpersonal problems and problems with the law. The goals of treatment are to reduce the frequency and severity of the client’s explosive outbursts and associated anxiety, without intolerable treatment-related side effects, and for the client to maintain his sobriety, as ordered by the court, and ultimately, to improve the client’s functioning and interpersonal relationships.
The treatment plan is to begin oxcarbazepine 300 mg orally, twice a day, and to gradually increase the dose until it is within the targeted therapeutic range of 1200 mg to 2400 mg per day. Additionally, the client will meet for weekly one-hour sessions for psychotherapy and motivational interviewing.
While research supports the use and efficacy of antidepressants such as selective serotonin reuptake inhibitors as first-line psychopharmacologic treatment for IED, the client has previously had two trials of different classes of antidepressants with no response to therapy. Research also supports the use of mood stabilizers, specifically oxcarbazepine and carbamazepine, in the treatment of impulsive disorders such as IED (Coccaro, 2010, 2018; Harvard Health Publishing, 2019). Research supports the use of psychotherapy such as cognitive behavioral therapy (CBT) to treat IED, suggesting that combination therapy with medication and CBT is associated with improved client outcomes (Coccaro, 2010, 2018; Harvard Health Publishing, 2019) . A review of research published by Harvard Health Publishing (2019) suggests CBT that combines coping skills training, cognitive restructuring, and relaxation training is a promising approach to the treatment of clients with IED. Research by Ubaidi (2017) supports the use of motivational interviewing as an effective intervention to elicit positive behavioral changes. CBT and motivational interviewing can also target anxiety and SUD, and mood stabilizers such as oxcarbazepine can treat bipolar disorder (Coccaro, 2010, 2018; Harvard Health Publishing, 2019; Stahl, 2017; Wheeler, 2014).
If the client is to be prescribed a mood stabilizer such as oxcarbazepine, he will require routine testing of serum levels to ensure the drug levels are within the therapeutic range. For example, if the client is prescribed oxcarbazepine as part of his treatment plan, he will require routine testing of plasma levels of the oxcarbazepine metabolite, 10-hydoroxycarbazepine, to determine if his oxcarbazepine level is within the therapeutic range. A plasma level that is below the therapeutic range of 8.0 to 35.0 mcg/mL is unlikely to achieve a therapeutic response, while a plasma level above the therapeutic range can lead to toxicity (Pagana & Pagana, 2018; Stahl, 2017).
References
American Nurses Association. (2014). Psychiatric-mental health nursing: Scope and standards of practice (2nd ed.). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2019). Seidel's guide to physical examination (9th ed.). St. Louis, MO: Elsevier Mosby.
Coccaro, E. F. (2010). A family history study of intermittent explosive disorder. Journal of Psychiatric Research, 44(15), 1101–1105. doi:10.1016/j.jpsychires.2010.04.006
Coccaro, E. F., Fridberg, D. J., Fanning, J. R., Grant, J. E., King, A. C., & Lee, R. (2016). Substance use disorders: Relationship with intermittent explosive disorder and with aggression, anger, and impulsivity. Journal of Psychiatric Research, 81, 127–132. doi:10.1016/j.jpsychires.2016.06.011
Coccaro, E. (2018). Intermittent explosive disorder in adults: Treatment and prognosis. In J. A. Melin (Ed.), UpToDate. Retrieved December 14, 2019, from https://www.uptodate.com/contents/intermittent-explosive-disorder-in-adults-treatment-and-prognosis
Harvard Health Publishing. (2019). Treating intermittent explosive disorder. Retrieved December 14, 2019, from https://www.health.harvard.edu/mind-and-mood/treating-intermittent-explosive-disorder
Marcogliese, E. D., & Vandyk, A. (2019). Mental health nurses’ knowledge of entry-to-practice competencies in psychiatric care. Journal of Continuing Education in Nursing, 50(7), 325–330. doi:10.3928/00220124-20190612-08
Mason, B. L., Brown, E. S., & Croarkin, P. E. (2016). Historical underpinnings of bipolar disorder diagnostic criteria. Behavioral Sciences (Basel, Switzerland), 6(3), 14. doi:10.3390/bs6030014
McAllister, M., Happell, B., & Flynn, T. (2014). Learning essentials: What graduates of mental health nursing programmes need to know from an industry perspective. JOURNAL OF CLINICAL NURSING, 23(23–24), 3449–3459. doi:10.1111/jocn.12594
Pagana, K. D., & Pagana, T. J. (2018). Mosby's manual of diagnostic and laboratory tests (6th ed.). St. Louis, Mo.: Elsevier.
Post, R. M., Altshuler, L., Kupka, R., McElroy, S. L., Frye, M. A., Rowe, M., … Nolen, W. A. (2015). Multigenerational positive family history of psychiatric disorders is associated with a poor prognosis in bipolar disorder. The Journal of Neuropsychiatry and Clinical Neurosciences, 27(4), 304–310. doi:10.1176/appi.neuropsych.14080204
Serre, F., Fatseas, M., Swendsen, J., & Auriacombe, M. (2017). How psychiatric comorbidity and mood states influence craving and substance use in daily life? An ecological momentary assessment study in patients with alcohol, tobacco, cannabis and heroin use disorders. Drug and Alcohol Dependence, 171, e187. doi:10.1016/j.drugalcdep.2016.08.513
Stahl, S. M. (2017). Stahl’s essential psychopharmacology: Prescriber’s guide (6th ed.). New York, NY: Cambridge University Press.
Ubaidi, B. (2017). Motivational Interviewing Skills: A tool for healthy behavioral changes. Journal of Family Medicine and Disease Prevention, 3(4). doi:10.23937/2469-5793/1510069
Wheeler, K. (2014). Psychotherapy for the advanced practice psychiatric nurse: A how-to guide for evidence-based practice (2nd ed.). New York, NY: Springer Publishing Company.
Zolezzi, M., Abdulrhim, S., Isleem, N., Zahrah, F., & Eltorki, Y. (2017). Medical comorbidities in patients with serious mental illness: A retrospective study of mental health patients attending an outpatient clinic in Qatar. Neuropsychiatric Disease and Treatment, Volume 13, 2411–2418. doi:10.2147/NDT.S141448
Appendix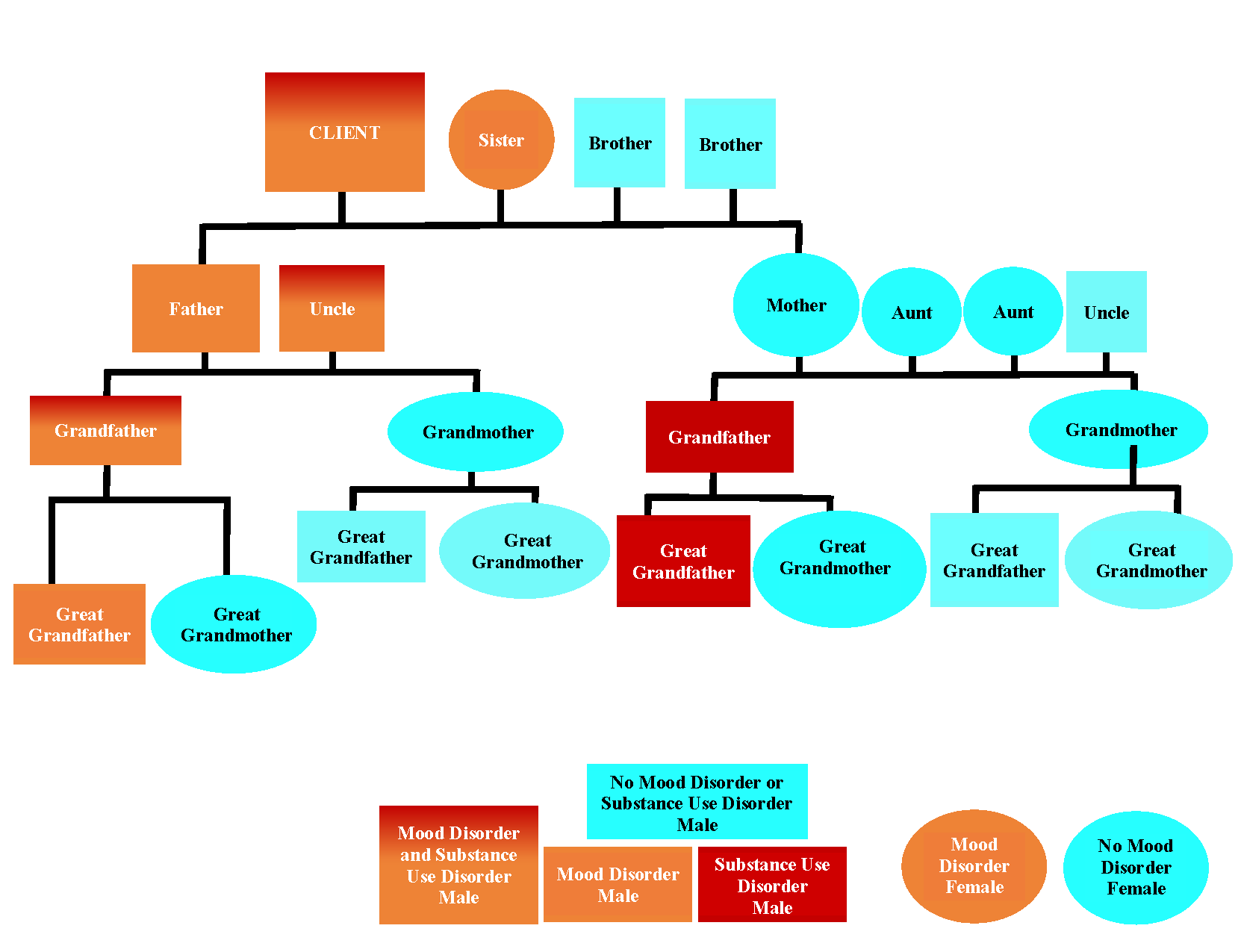
Client Genogram
Expert Solution
Need this Answer?
This solution is not in the archive yet. Hire an expert to solve it for you.







